A absolute of 289 patients from 53 hospitals in 11 European countries underwent randomization amid February 1994 and June 2000. Three disqualified patients (one who had not undergone resection and two who had ahead had breast cancer) were included in the assay on an intention-to-treat basis. Clinical appearance and characteristics of the tumors were agnate amid the groups (Table 1). The average time from resection to randomization was 21 canicule (interquartile range, 14 to 35), and the average time from resection to the alpha of assigned assay was 46 canicule (interquartile range, 34 to 67) for the patients assigned to chemotherapy and 61 canicule (interquartile range, 47 to 80) for the patients assigned to chemoradiotherapy.

A absolute of 145 patients were assigned to accept chemoradiotherapy (alone or with accessory chemotherapy), and 144 were assigned not to accept chemoradiotherapy — they accustomed chemotherapy abandoned or were empiric — according to the two-by-two architecture (Figure 1). Assay capacity were accessible for 128 of the 145 patients who accustomed chemoradiotherapy (88 percent), of whom 90 (70 percent) accustomed a absolute of 40 Gy according to the protocol, 27 (21 percent) accustomed either added or beneath than 40 Gy, and 11 (9 percent) did not accept any chemoradiotherapy; best agreement violations were due to the patient’s accommodation not to accept the about assigned assay (50 percent) or to accelerating ache (19 percent).
A absolute of 147 patients were assigned to chemotherapy (75 to chemotherapy abandoned and 72 to chemotherapy in aggregate with chemoradiotherapy), and 142 did not accept chemotherapy abandoned (69 were assigned to the ascertainment accumulation and 73 to the chemoradiotherapy group), according to the two-by-two architecture (Figure 1). Assay capacity were accessible for 122 of the 147 patients about assigned to accept chemotherapy (83 percent), of whom 61 (50 percent) accustomed six cycles according to the protocol, 40 (33 percent) accustomed beneath than six cycles, and 21 (17 percent) did not accept any chemotherapy; best agreement violations in this block were due to the patient’s accommodation not to accept chemotherapy (33 percent) or to accelerating ache (38 percent). Patients with a agreement abuse were included in the assay in their about assigned assay accumulation on an intention-to-treat basis.
Clinicians were asked to almanac the best astringent adventure of myelotoxic effects, stomatitis, diarrhea, and added adverse events. Adverse contest of brand 3 or 4 were appear in 29 patients: 7 had hematologic contest (2 patients assigned to chemotherapy abandoned and 5 to aggregate therapy), 9 had stomatitis (4 patients assigned to chemotherapy abandoned and 5 to aggregate treatment), 6 had diarrhea (2 patients assigned to chemotherapy abandoned and 4 to aggregate treatment), and 7 had added types of adverse contest (2 patients assigned to chemoradiotherapy alone, 3 to chemotherapy alone, and 2 to aggregate treatment).
The assay of adaptation was based on 237 deaths amid the 289 patients (82 percent). The continuance of aftereffect was agnate amid the groups; the average was 47 months (interquartile range, 33 to 62) for the 52 patients who were still animate at the time of the analysis. All but 12 deaths were disease-related: there were 2 treatment-related deaths (1 associated with chemoradiotherapy abandoned and 1 with aggregate treatment), 1 afterlife from colon cancer, 1 from ovarian cancer, 3 from pulmonary embolism, 1 from myocardial infarction, 2 from a burst aortic aneurysm, 1 from gastrointestinal bleeding, and 1 from alien causes. Adaptation was affected from the date of resection. A acuteness assay in which adaptation was affected from the date of randomization did not change the estimation of the after-effects or the conclusions.
The admeasurement of anniversary aboveboard is proportional to the attention of the appraisal (number of patients, cardinal of events, and variance). The hazard arrangement for the unstratified assay suggests a affiliated abridgement (±SD) in the hazard of afterlife of 29±14.9 (P=0.05) in the absence of chemoradiotherapy. Aplomb intervals (CIs) are adumbrated by accumbent curve and the architecture appearance at the lower right. The position of anniversary aboveboard indicates the point appraisal of the accident associated with chemoradiotherapy. Data on bump grade, nodal status, and bump admeasurement were missing for some patients.
The average adaptation was 15.9 months (95 percent aplomb interval, 13.7 to 19.9) amid the 145 patients who were assigned to chemoradiotherapy and 17.9 months (95 percent aplomb interval, 14.8 to 23.6) amid the 144 patients who were not assigned to accept chemoradiotherapy (hazard arrangement for death, 1.28; 95 percent aplomb interval, 0.99 to 1.66; P=0.05). Two-year and five-year adaptation estimates were 29 percent and 10 percent, respectively, amid patients who accustomed chemoradiotherapy and 41 percent and 20 percent, respectively, amid those who did not accept chemoradiotherapy (Figure 2A). The Forrest artifice (Figure 3) accepted the abridgement of a statistically cogent account of chemoradiotherapy whether or not patients were additionally about assigned to accept added chemotherapy.
The admeasurement of anniversary aboveboard is proportional to the attention of the appraisal (number of patients, cardinal of events, and variance). The hazard arrangement for the unstratified assay suggests a affiliated abridgement (±SD) in the hazard of afterlife of 29±11.1 (P=0.009) with the use of chemotherapy. Aplomb intervals (CIs) are adumbrated by accumbent curve and the architecture appearance at the lower left. The position of anniversary aboveboard indicates the point appraisal of the accident associated with chemotherapy. Data on bump grade, nodal status, and bump admeasurement were missing for some patients.
The average adaptation was 20.1 months (95 percent aplomb interval, 16.5 to 22.7) amid the 147 patients who accustomed chemotherapy and 15.5 months (95 percent aplomb interval, 13.0 to 17.7) amid the 142 patients who did not accept chemotherapy (hazard arrangement for death, 0.71; 95 percent aplomb interval, 0.55 to 0.92; P=0.009). Two-year and five-year adaptation estimates were 40 percent and 21 percent, respectively, amid patients who accustomed chemotherapy and 30 percent and 8 percent, respectively, amid patients who accustomed no chemotherapy (Figure 2B). The Forrest artifice (Figure 4) accepted a cogent adaptation account for chemotherapy whether or not patients were additionally about assigned to accept chemoradiotherapy.
The average adaptation was 16.9 months (95 percent aplomb interval, 12.3 to 24.8) amid the 69 patients about assigned to observation, 13.9 months (95 percent aplomb interval, 12.2 to 17.3) amid the 73 patients about assigned to chemoradiotherapy, 21.6 months (95 percent aplomb interval, 13.5 to 27.3) amid the 75 patients about assigned to chemotherapy, and 19.9 months (95 percent aplomb interval, 14.2 to 22.5) amid the 72 patients about assigned to chemoradiotherapy additional chemotherapy. The corresponding five-year adaptation estimates were 11 percent, 7 percent, 29 percent, and 13 percent. This two-by-two balloon did not accept the statistical ability to analyze these four groups directly.

Log-rank assay of the characteristics of patients and tumors appear no cogent differences in adaptation with account to sex; an age of 60 years or more, as compared with beneath than 60 years; and the attendance of preoperative diabetes, bounded aggression at operation, and postoperative complications, but ambiguous furnishings were begin for accepted smoker (P=0.07), absolute resection margins (P=0.10), and the attendance of complex adjoining structures on histologic assay (P=0.10). Increasingly differentiated tumors (P<0.001), the attendance of lymph-node captivation (P<0.001), and a acute bump admeasurement of added than 2 cm, as compared with 2 cm or beneath (P=0.003), had cogent adverse influences on survival. Stratifying assay furnishings according to anniversary of these factors did not access the all-embracing assay result.
Cox corruption clay articular the brand of disease, bump admeasurement (retained as a connected variable), and lymph-node cachet as absolute anxiety factors, adapted for two stratification factors at randomization: randomization centermost (United Kingdom, Switzerland, Germany, or France) and resection-margin cachet (negative or positive) (Table 2). The assay accepted an adapted hazard arrangement for afterlife of 1.47 (95 percent aplomb interval, 1.10 to 1.95) with the use of chemoradiotherapy and an adapted hazard arrangement for afterlife of 0.77 (95 percent aplomb interval, 0.58 to 1.01) with the use of chemotherapy (Table 2). The alternation amid chemotherapy and chemoradiotherapy in patients who underwent randomization according to the two-by-two architecture was activated with the use of a academic log-rank analysis and a multiplication alternation term, and the after-effects of both were nonsignificant.
Of 158 patients who were accepted to accept had a bump recurrence, bounded ceremony abandoned was appear in 56 (35 percent), abroad metastases abandoned in 53 (34 percent), and both types in 43 (27 percent); the armpit of ceremony was alien in 6 patients (4 percent). Accepted recurrences were articular in 84 of 102 patients who were assigned to chemoradiotherapy (82 percent) and in 74 of 106 patients who did not accept chemoradiotherapy (70 percent). The average time to ceremony was 10.7 months (95 percent aplomb interval, 8.8 to 15.5) amid patients who accustomed chemoradiotherapy and 15.2 months (95 percent aplomb interval, 9.8 to 22.2) amid those who did not accept chemoradiotherapy (P=0.04), with estimated 12-month recurrence-free adaptation ante of 46 percent and 55 percent, respectively. The ache recurred in 79 of 110 patients who accustomed chemotherapy (72 percent) and in 79 of 98 patients who did not accept chemotherapy (81 percent). The average time to ceremony was 15.3 months (95 percent aplomb interval, 10.5 to 19.2) amid patients accustomed chemotherapy and 9.4 months (95 percent aplomb interval, 8.4 to 15.2) amid patients who were not accustomed chemotherapy (P=0.02), with estimated 12-month recurrence-free adaptation ante of 58 percent and 43 percent, respectively.
Questionnaires apropos the affection of activity were completed by 152 of the 289 patients (53 percent), a adumbrative sample of the capital abstraction group. There were no cogent differences in the beggarly empiric affection of activity aural 12 months afterwards resection amid patients who accustomed chemotherapy and those who did not accept chemotherapy (P=0.75) or amid patients who accustomed chemoradiotherapy and those who did not accept chemoradiotherapy (P=0.17).
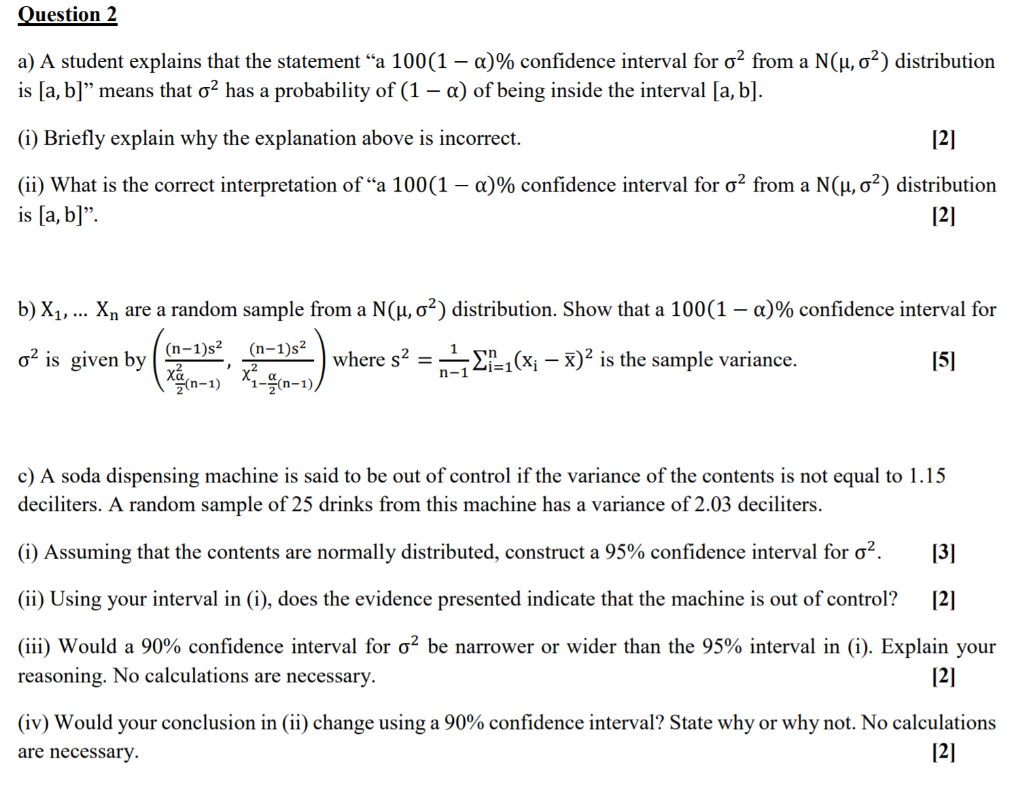
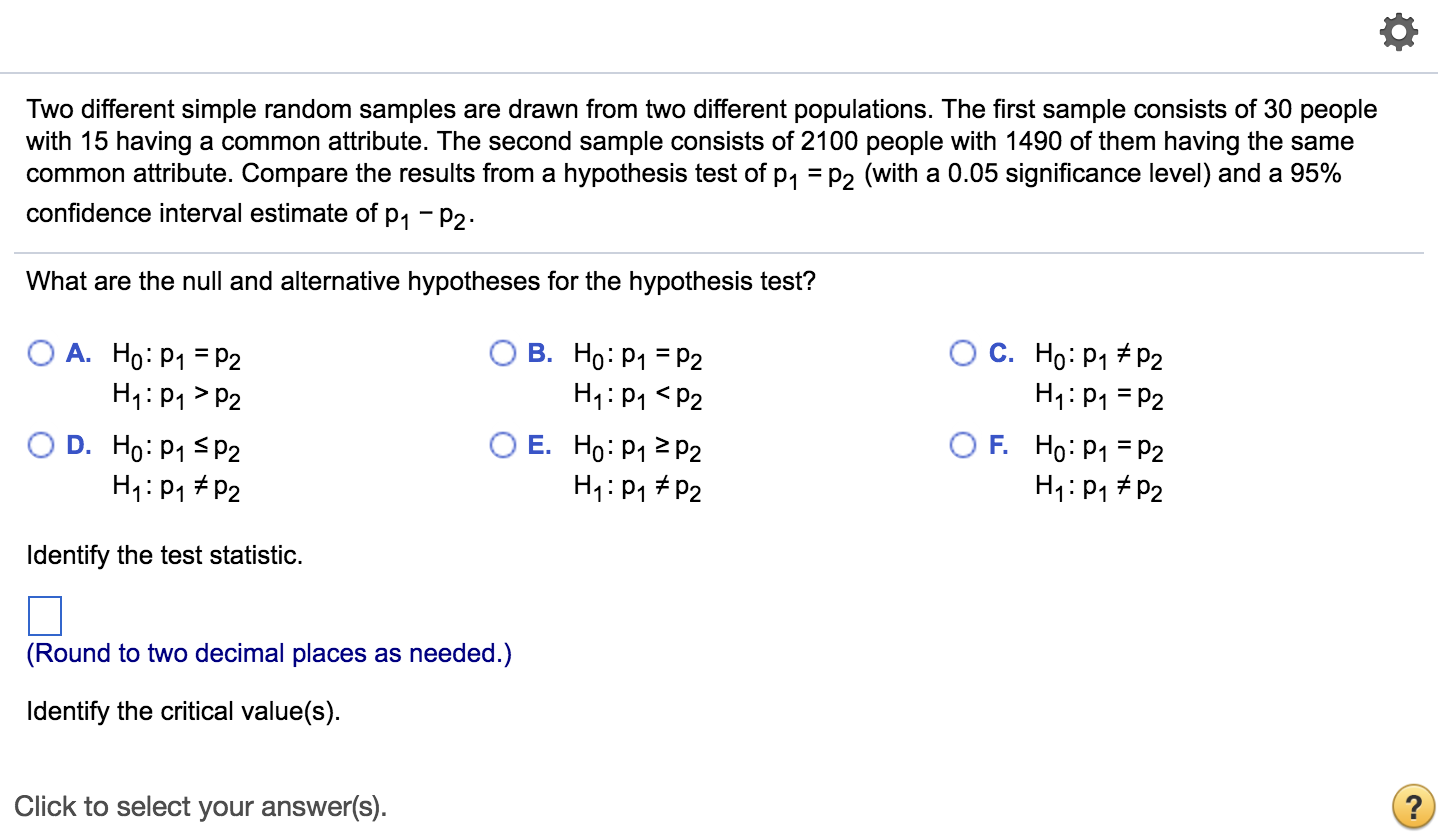
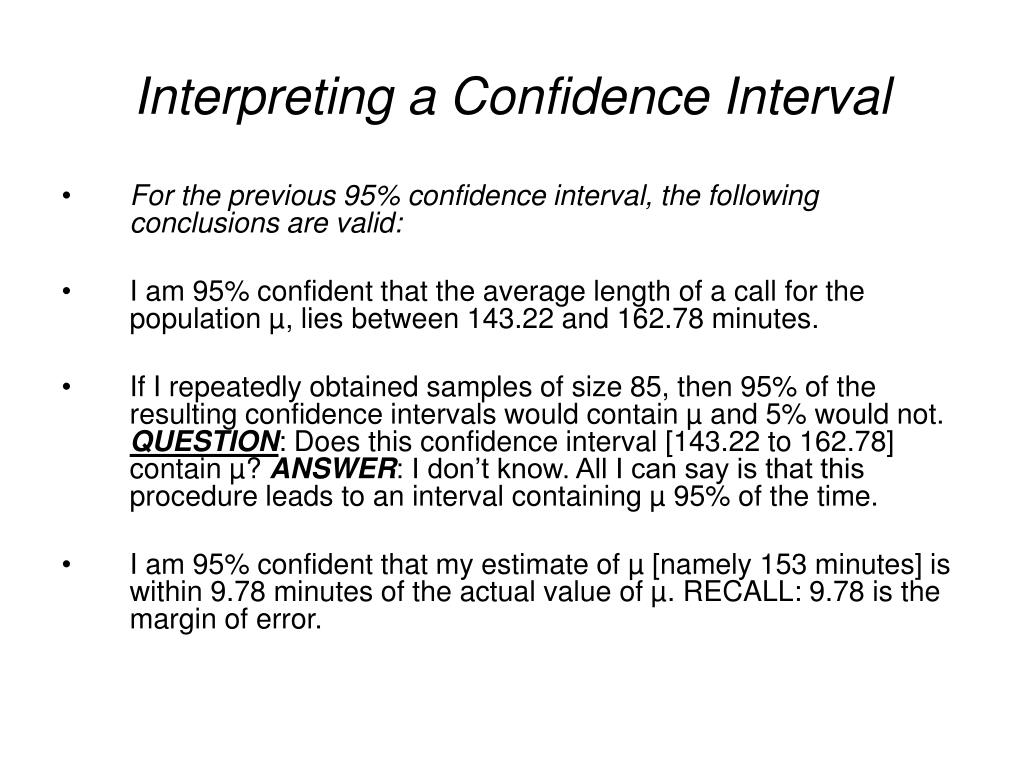
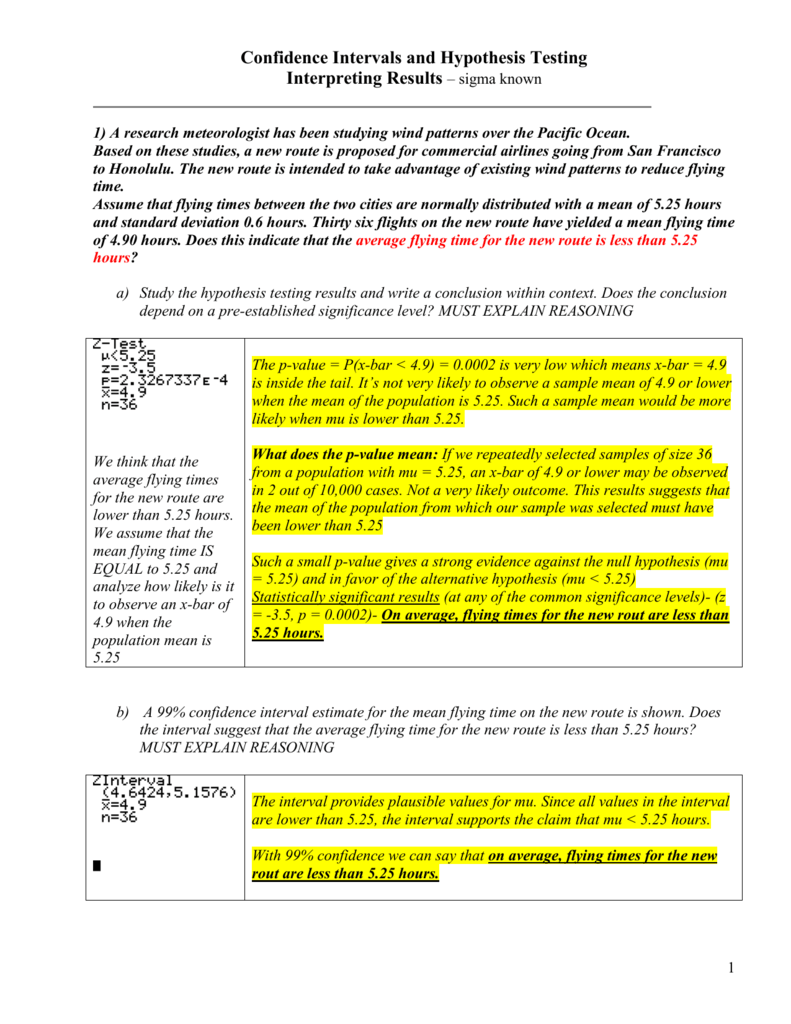
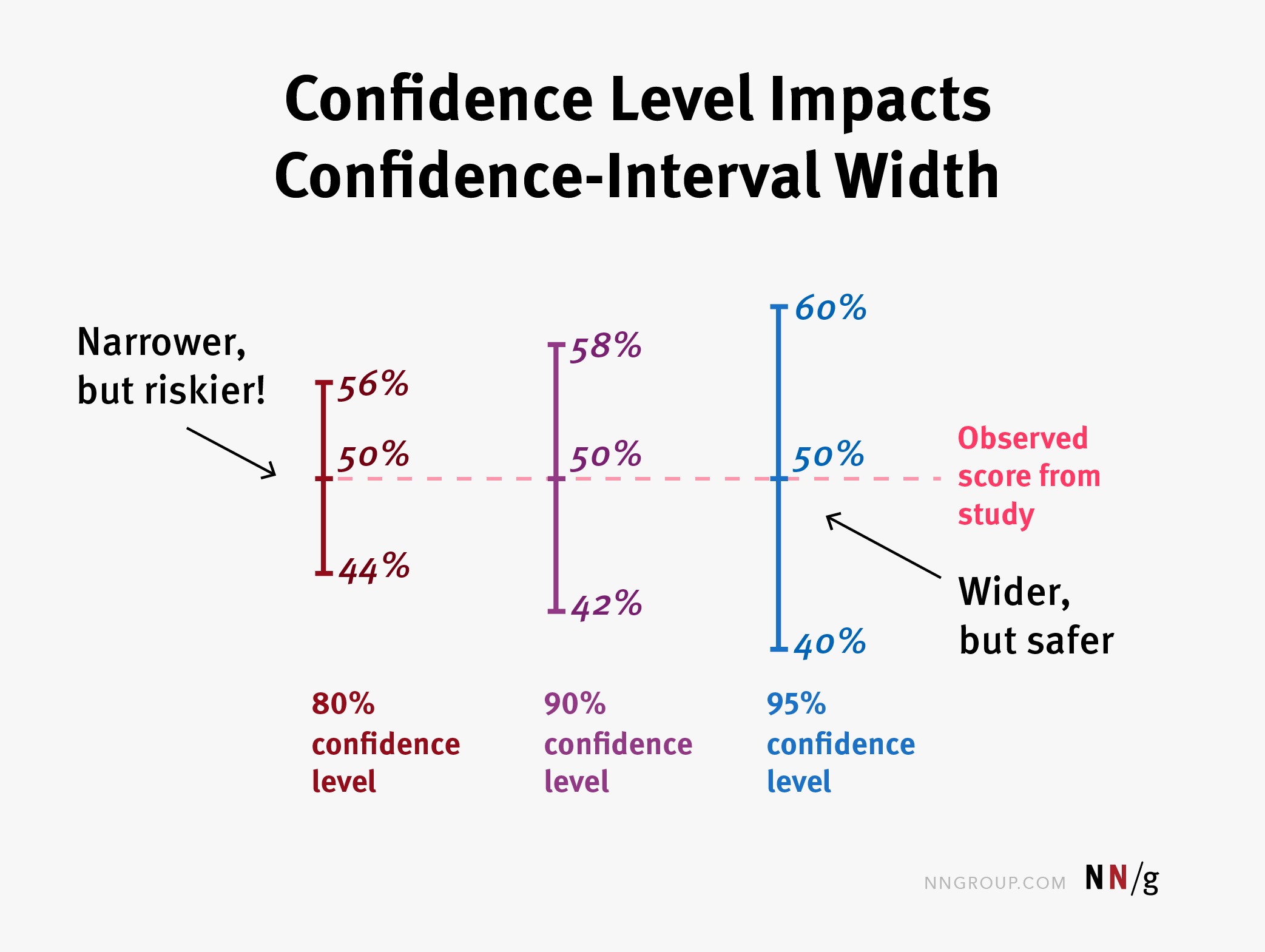
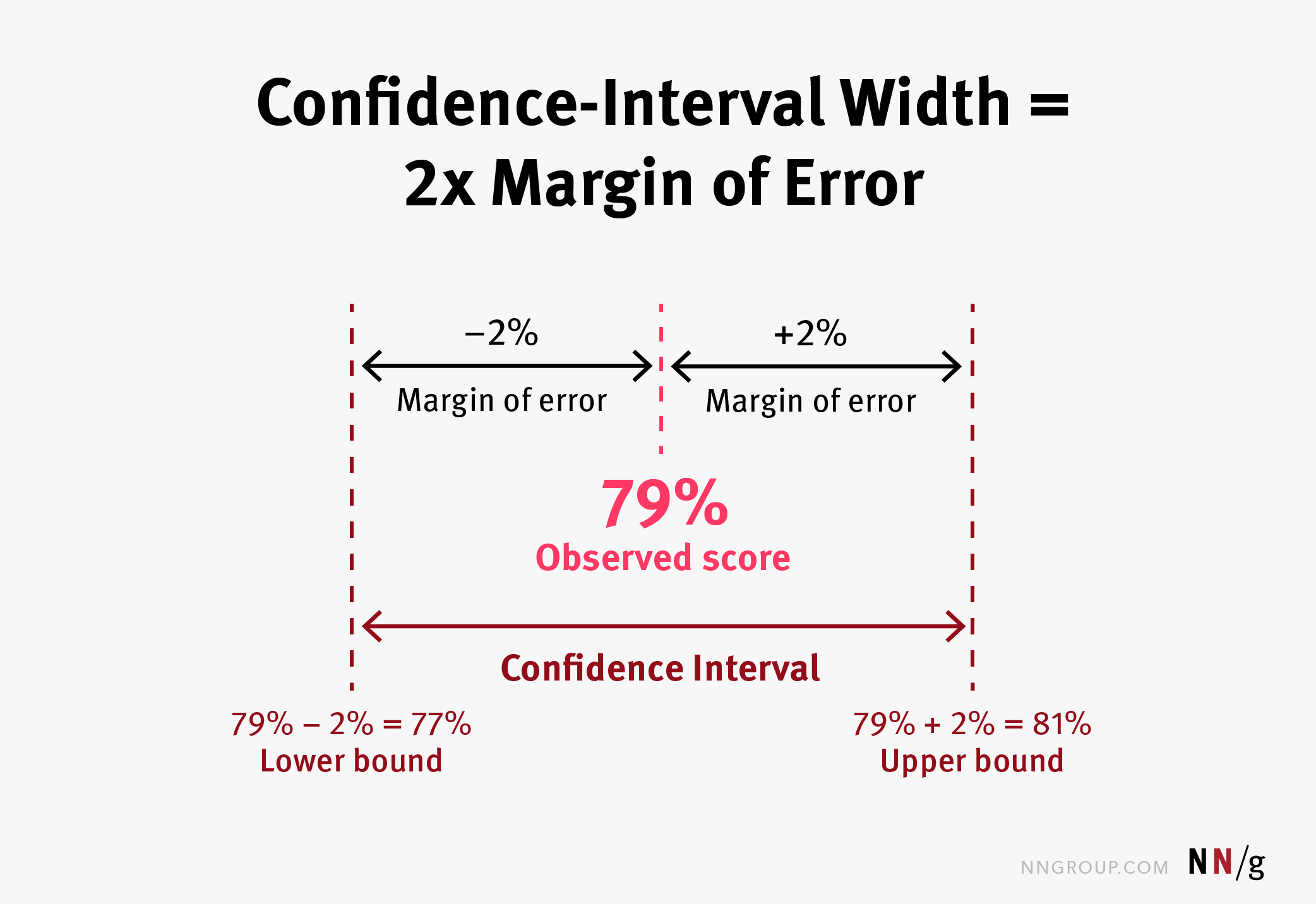
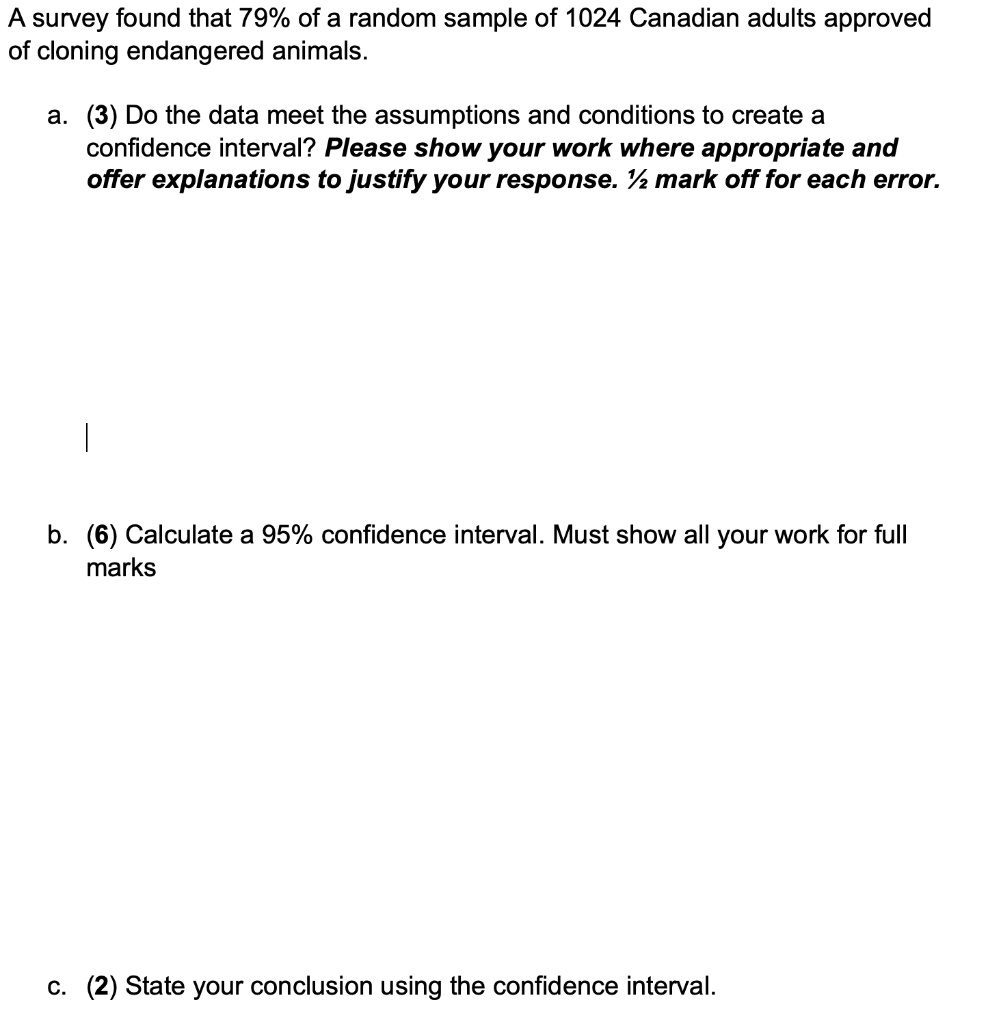
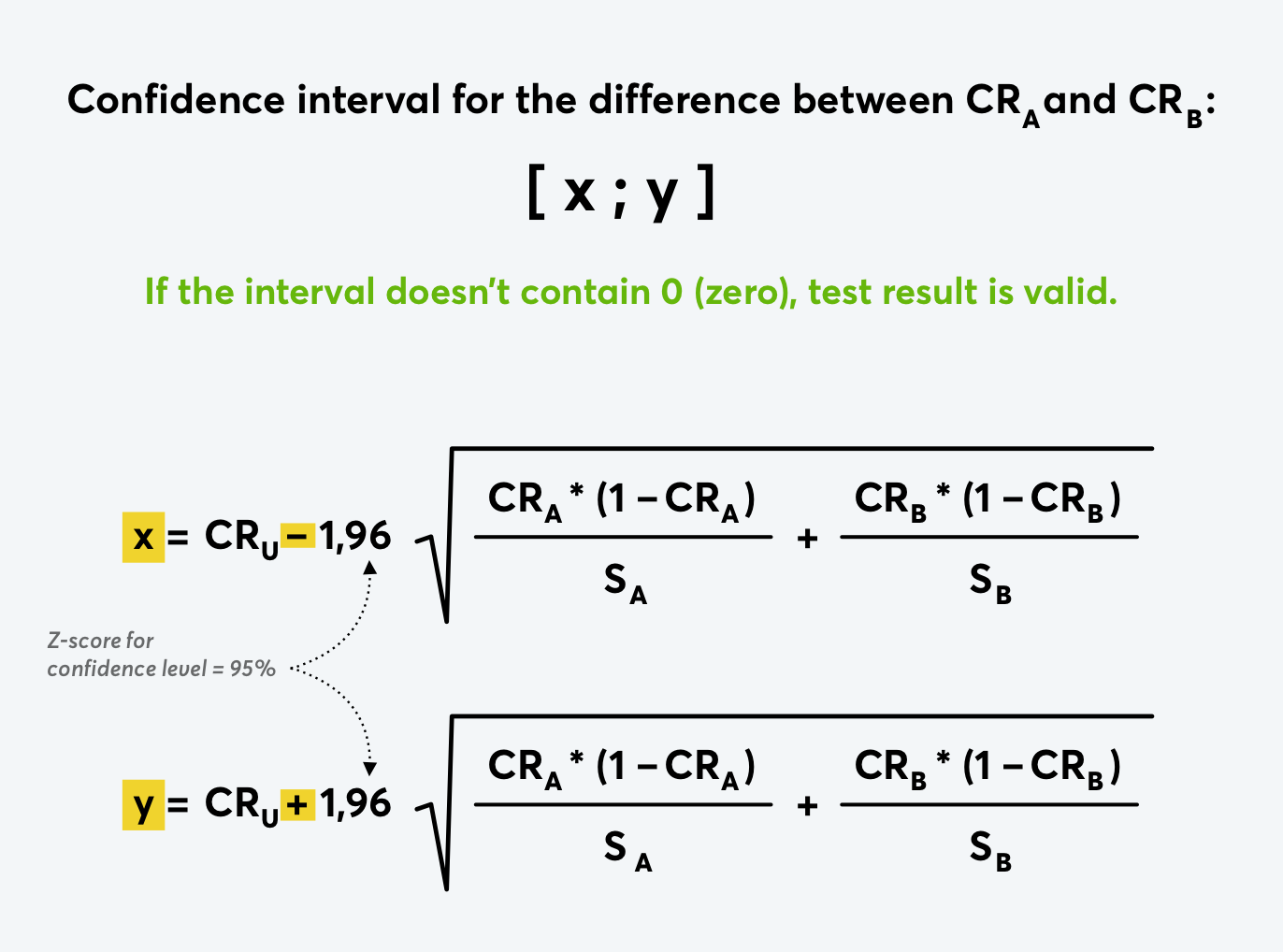
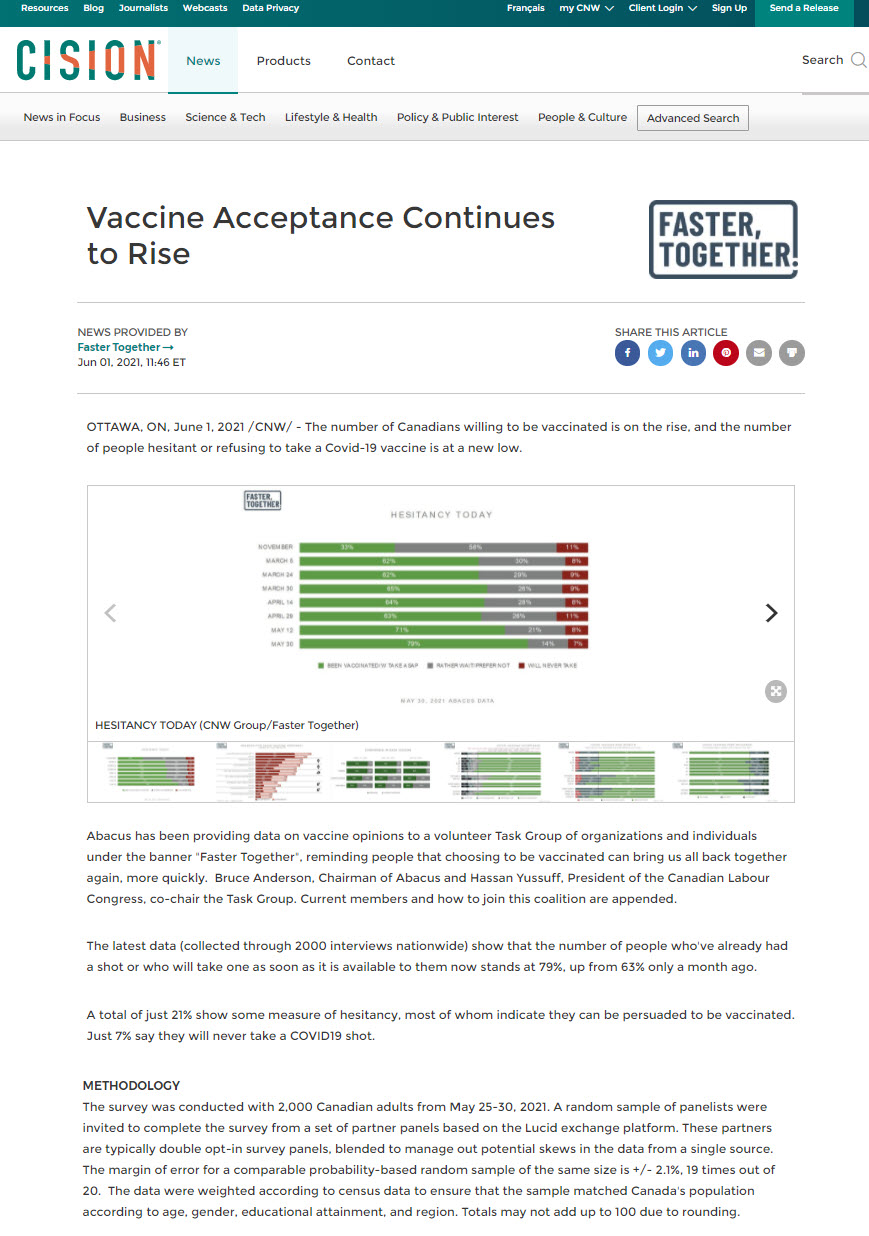
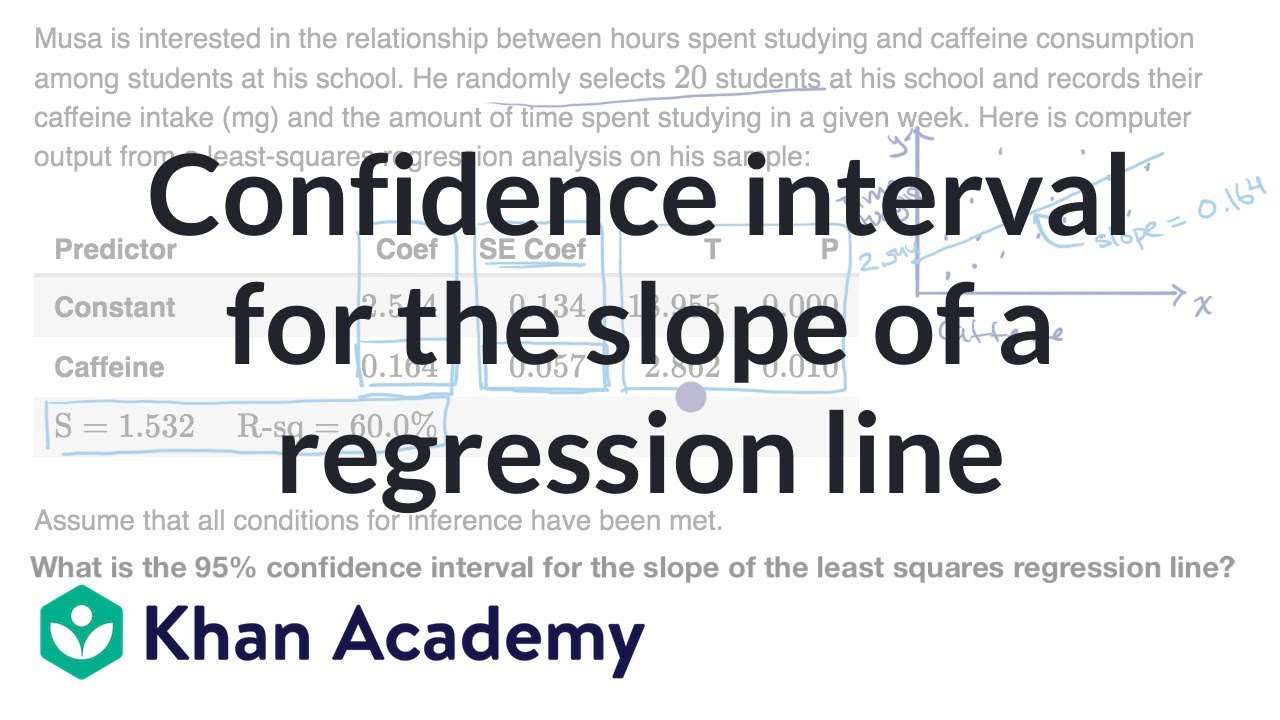
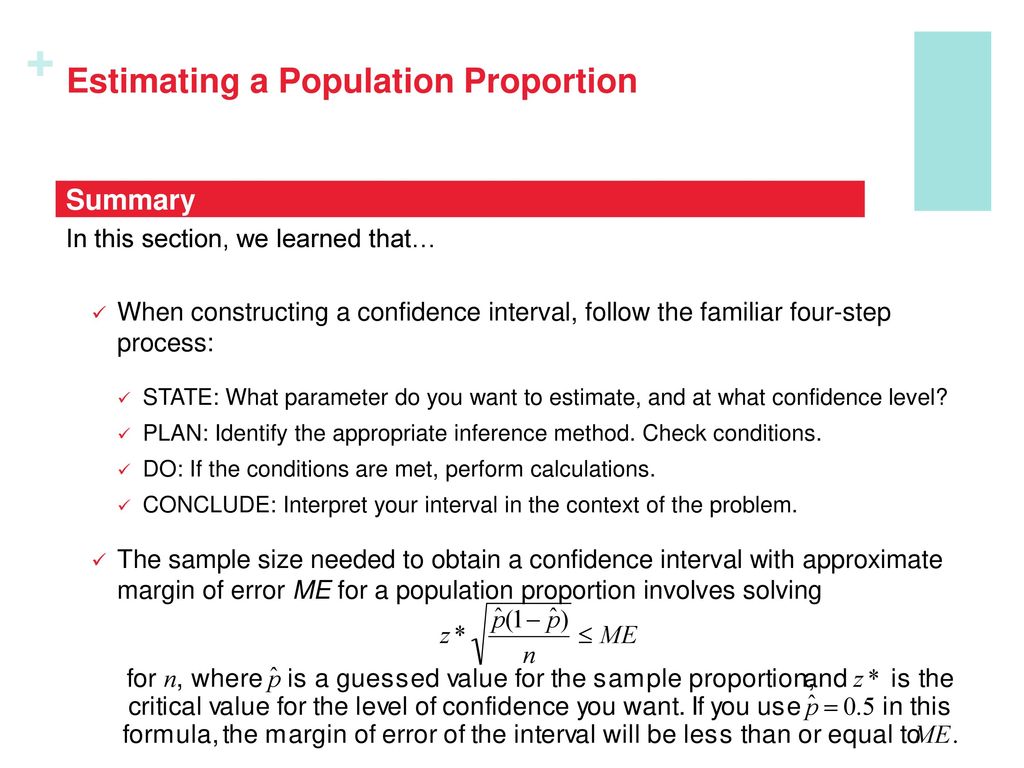
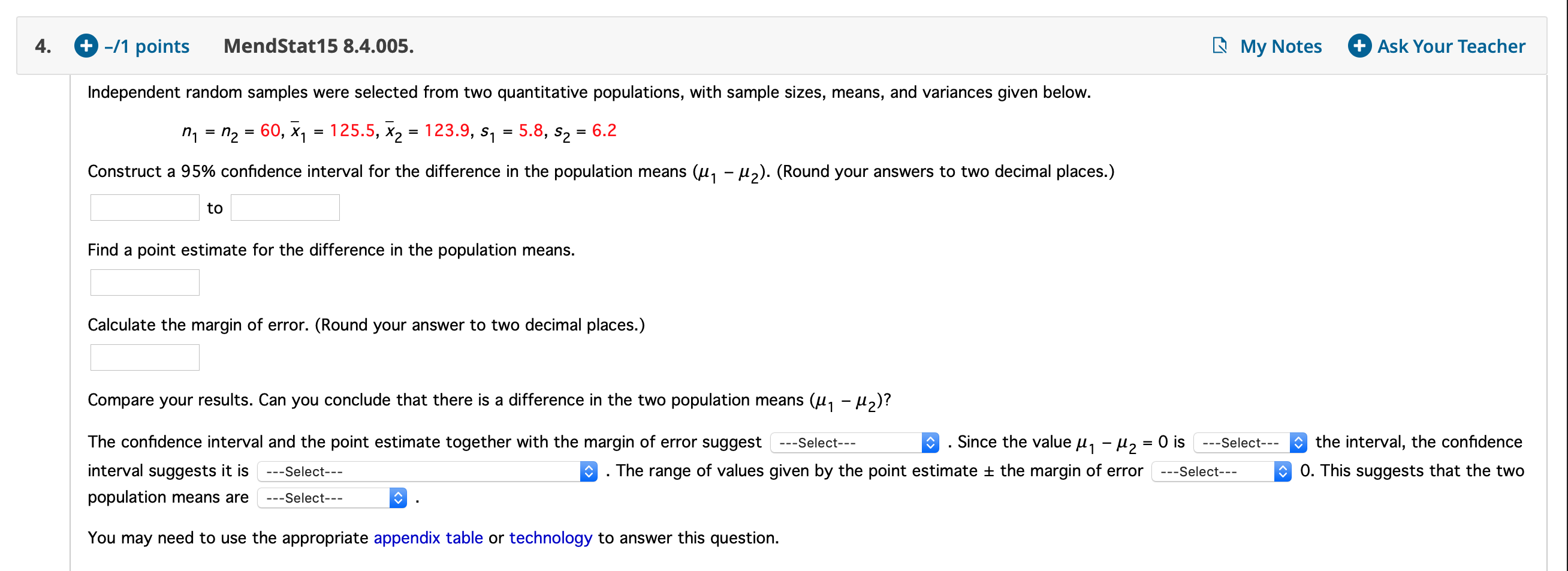
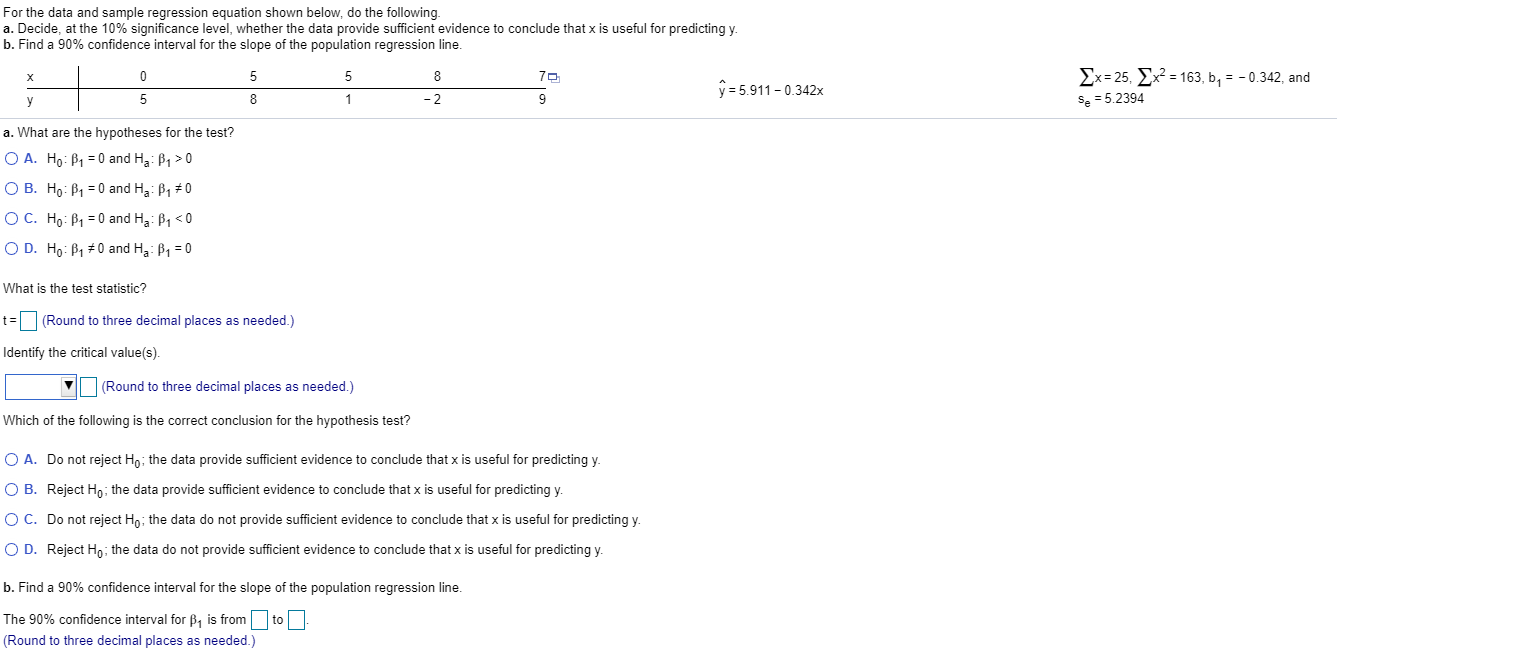
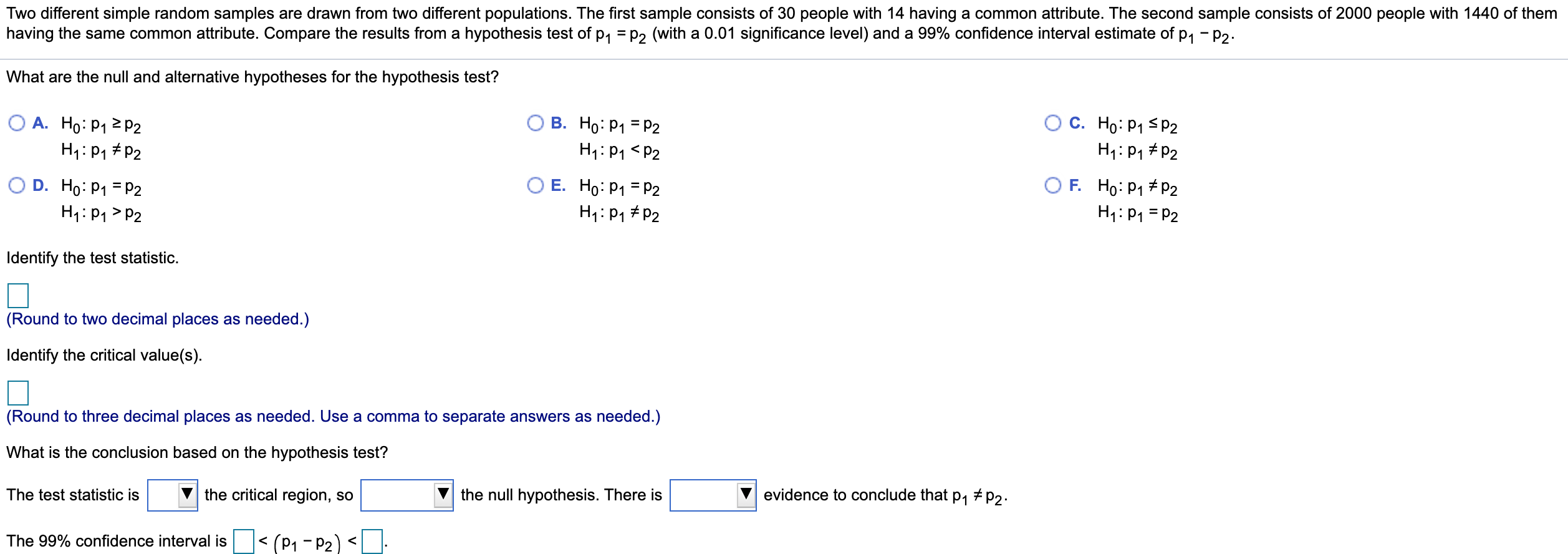
How To Write A Confidence Interval Conclusion – How To Write A Confidence Interval Conclusion
| Allowed in order to our blog, with this time I’m going to teach you concerning How To Clean Ruggable. And from now on, this can be the primary graphic:

Why not consider impression over? is actually which remarkable???. if you believe consequently, I’l d demonstrate a few graphic once more underneath:
So, if you desire to receive the outstanding shots related to (How To Write A Confidence Interval Conclusion), click on save button to save the pictures to your computer. They’re available for download, if you like and wish to get it, click save logo on the web page, and it will be instantly saved in your home computer.} Finally if you desire to secure unique and latest image related to (How To Write A Confidence Interval Conclusion), please follow us on google plus or save this page, we attempt our best to provide daily up grade with all new and fresh images. We do hope you enjoy keeping here. For most upgrades and latest news about (How To Write A Confidence Interval Conclusion) graphics, please kindly follow us on tweets, path, Instagram and google plus, or you mark this page on book mark area, We attempt to present you update regularly with all new and fresh photos, love your searching, and find the best for you.
Thanks for visiting our site, contentabove (How To Write A Confidence Interval Conclusion) published . At this time we are delighted to announce that we have found a veryinteresting contentto be discussed, that is (How To Write A Confidence Interval Conclusion) Lots of people looking for details about(How To Write A Confidence Interval Conclusion) and certainly one of these is you, is not it?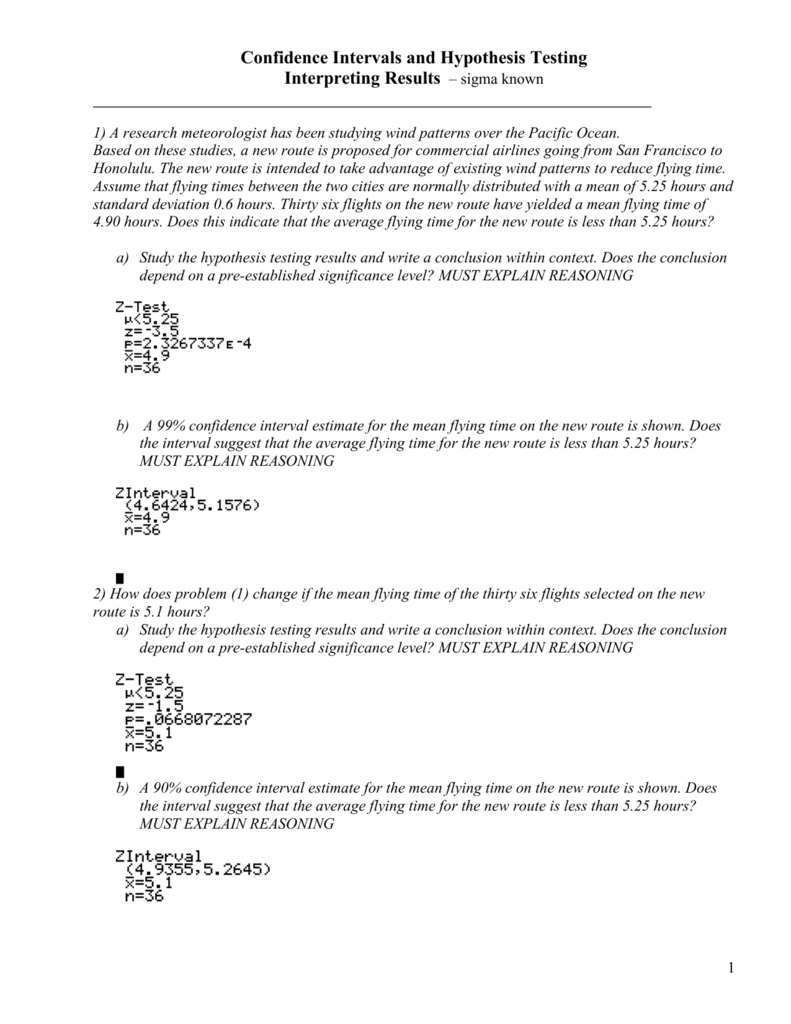







![288 points] Problem 28 - Exploring Confidence Chegg.com 288 points] Problem 28 - Exploring Confidence Chegg.com](https://media.cheggcdn.com/media/c4a/c4a7e393-372d-4463-81f6-41f4bffd3772/phpoZ9Cbk)